A long-time Port McNeill doctor says the North Island has become “invisible” to provincial government health authorities. Dr. Prean Armogam, a South African-born and educated physician, has been practicing in this North Island community since 2004. He said calls to fix failing health care in the region have gone largely ignored by Island Health.
“We need predictable access to acute care and predictable messaging to the public,” Dr. Armogam told VanIsleNews in an interview.
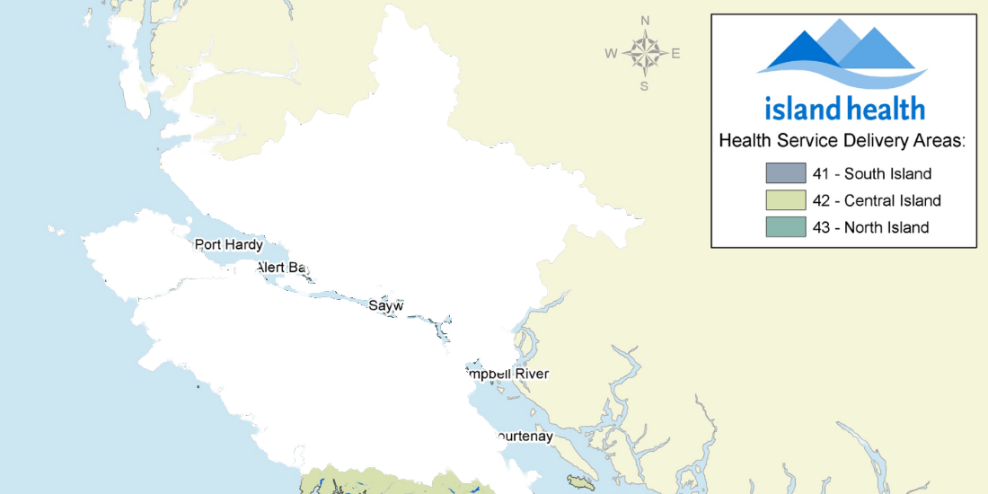
He and other healthcare workers have been asking Island Health to consolidate acute emergency care at the Port McNeill Hospital, while having primary care treatment available in Port Hardy, Alert Bay, Sointula and Port Alice.
They’ve suggested it’s the best use of limited resources and an efficient way to improve healthcare delivery.
Their suggestions are not new.
A 2011 report by Novatone Consulting prepared for Island Health recommended temporarily consolidating emergency care in the region until a sustainable model is found. However, according to Dr. Armogam, Island Health buried the report.
Island Health is now supposed to be providing emergency care services at both the Port Hardy and Port McNeill hospitals. This approach isn’t working.
Dr. Armogram, who resigned as Island Health Medical Health Director for Mount Waddington-Strathcona in 2021 because he was frustrated by the lack of leadership, said the current model is badly broken.
In 2022, staffing shortages forced Island Health to close the emergency room in Port Hardy 30 times and the one in Port McNeill 10 times. In the latest incident, on November 25, 2022, a patient who complained of chest pains collapsed on the floor outside the closed Port Hardy Hospital ER department. Staff called BC Ambulance Service (BCAS,) which said an ambulance from Port McNeill, 43 km away, was being sent.
It was a gong show. While waiting, a nurse helped the patient onto a gurney and took their vitals. When no ambulance arrived, the staff called the BC Ambulance Service again. They were told that because medical staff had intervened, it was assumed that the hospital had taken control of the situation. Port Hardy hospital staff said they were told extra steps would be needed to make a hospital-to-hospital transfer.
That’s just one example of the North Island healthcare crisis. Patient loads are heavy for North Island doctors and nurses.
Dr. Armogam works 16 to 18 hours a day, serving more than 2,800 patients from his private clinic in Port McNeill. He also spends many days on the road visiting patients in Sointula, Zeballos, and other outlying communities.
Dr. Armogam acknowledged it’s not “sustainable on a personal level. Medical staff are burning out…We need five more physicians in Port McNeil.”
It’s not only people’s health being affected. “My fear is that the situation will get worse, and people won’t come to the North Island to live and work,” said Dr. Armogam.
A revolving door of physicians, along with two-year contracts, has partially helped with the healthcare crisis on the North Island.
Dr. Armogam said his relationship with Island Health has soured because he’s outspoken. He’s speaking up because he wants the health authority to help medical staff serve the community better.
However, Island Health says the health authority is taking the situation on the North Island seriously.
“Island Health acknowledges this continues to be an extremely challenging time for everyone involved in the delivery of health care in the Mt. Waddington region, as well as for all the other communities we serve,” Island Health spokesperson said in an emailed response to VanIsle.News. “We recognize the need for predictability and stability in the delivery of emergency services as well,” spokesperson Andrew Leyne said in an email.
Leyne said the health authority has examined the Nov. 25 incident at the Port Hardy Hospital and is confident that the necessary clarifications and procedures have been implemented to prevent similar patient care confusion.
In early November, Island Health took part in a health summit for the Mt. Waddington region hosted by the Rural Coordination Centre of BC and is awaiting a follow-up report.
“The collaborative work undertaken by attendees representing partners from across the region will guide Island Health as we develop strategies to bring stability and predictability to service delivery in the region,” Leyne said.